|
03 November 2011
from
NWOTruth Website
Governments around the world have been trying to work with the
pharmaceutical industry to come up with (conventional) new ways to
tackle the growing “superbug” problem.
But an experimental new drug treatment
regime touted as a potential solution for superbugs has been exposed
as a complete failure, as those who receive it are five times more
likely to develop serious infections than those who are treated the
old way.
Professor David Neal from the University of Cambridge and his
colleagues at the school’s Addenbrooke Hospital evaluated 709
prostate cancer patients who were undergoing diagnosis surgery for
their conditions. One group received the typical
ciprofloxacin drug treatment, while
the other received an experimental combination of
co-amoxiclav and
gentamicin, which are two types of
antibiotics.
Published in the British Journal of Urology, their study
revealed that patients treated with co-amoxiclav and gentamicin have
a 500 percent
increased risk of developing serious infective
complications compared to patients given the typical drug
treatment.
While only 2.4 percent of the 454 patients in the ciprofloxacin
group developed infections, nearly 13 percent of patients in the co-amoxiclav/gentamicin
group ended up developing infections - and nearly five percent from
the latter group ended up back in the hospital with severe cases of
sepsis or septic shock.
“Any alteration to existing
departmental antibiotic policies should be linked to strong
clinical evidence,” commented Prof. Neal concerning the
findings.
“[S]uch changes may potentially
result in significant ill health and potential harm, as well as
the financial burden of treating new complications.”
The experimental switch was prompted by
new UK government guidelines which purported that ciprofloxacin
treatments were spurring increases in
Clostridium difficile infections.
While this is true, at least in part,
the government’s unfounded “solution” is an embarrassing indictment
of what happens when
the drug industry is entrusted with
finding fixes to the problems it played a role in creating.
Overprescribing and overuse of antibiotics like,
-
fluoroquinolones
-
cephalosporins
-
clindamycin
-
penicillins,
...among the general population has been
demonstrated as one of the
primary causes of superbug proliferation.
The overuse of antibiotics in agriculture to make livestock grow
more quickly is another primary cause.
Source
New Drugs Used to Tackle Superbugs...
"Increase Risk of Infection"
by Daily Mail Reporter
November 01, 2011
from
DailyMail Website
New drugs used to tackle hospital
superbugs can actually increase the risk of infection, researchers
warn. After certain surgeries, the number of infections in patients
given a new regime of drugs was higher than among those on the old
regime, a study found.
Of 709 patients undergoing a prostate cancer diagnosis operation,
those given the new course of antibiotics to fight infections
developed five times as many complications.
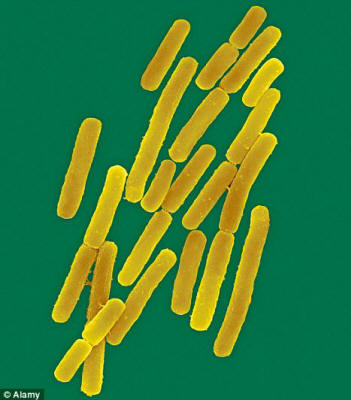
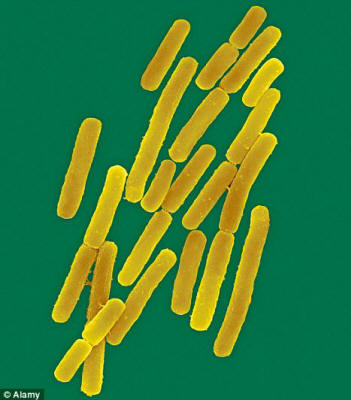
Clostridium difficile
New drugs make
infections more likely, new research suggests
These included a number of cases of
sepsis, in which the blood is overwhelmed by bugs, and one case of
septic shock needing emergency treatment to prevent heart failure.
Professor David Neal, researcher, said:
'Any alteration to existing
departmental antibiotic policies should be linked to strong
clinical evidence, because such changes may potentially result
in significant ill health and potential harm, as well as the
financial burden of treating new complications.'
Professor Neal's team at Addenbrooke's
Hospital, Cambridge, found that after a urological procedure to
diagnose prostate cancer, only 2.4 per cent of the 454 patients
treated with the standard drugs - ciprofloxacin - developed an
infective problem.
But 12.9 per cent given the new regime of prophylaxis with
coamoxiclav and gentamicin developed an infection in the same period
and twelve (4.7 per cent) were admitted for complications - seven of
whom suffered sepsis and one septic shock.
None of the patients on the original therapy had these very serious
complications and re-introducing the original regime led to a fall
in infective complications.
Professor Neal said:
'The change, based on national
guidance, reflected concerns C. difficile rates were being
driven by the widespread use of broad-spectrum antibiotics such
as ciprofloxacin.
'The new regime was introduced on the proviso that both the
hospital-acquired infection rates and post-operative infection
rates would be closely monitored.
'Given there were no cases of C.
difficile recorded in our study but post-operative infection
rates increased significantly the decision was taken to revert
back to the original regime.'

Infection control
A close up of a nurse
washing her hands in alcohol gel at a Yorkshire hospital
The researchers whose findings are
published in the British Journal of Urology International
said the antibiotic prophylaxis needs to reflect the local situation
both in terms of the organisms encountered and the local C. diff
rates.
Any changes also need to be subject to
frequent review.
Professor Neal said:
'Even though the procedure -
TRUSP Bx - is a common
urological procedure there are currently no national guidelines
regarding antibiotic prophylaxis and local protocols vary widely
across the UK.
'However, the importance of using prophylaxis for a biopsy, to
reduce the occurrence of infective complications following
surgery, has been well documented.
'This is the first study to compare the use of co-amoxiclav and
gentamicin with the use of ciprofloxacin for TRUSP Bx.
'Patients given the original ciprofloxacin regime experienced
significantly fewer infective complications than those on the
new regime and this audit study supports the use of locally
determined prophylactic regimes for this procedure.'
|