|
December 01, 2001
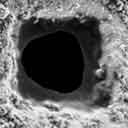
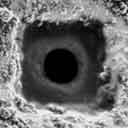
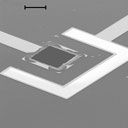
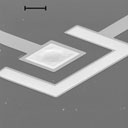
Above, left: In Langer's chip, medicine is stored beneath 50-micrometer squares of gold membrane (top). A small electric charge administered either remotely or via a small battery dissolves the gold cap, releasing the drug (bottom). Above, right: One prototype chip holds 100 drug-containing reservoirs (top). The circuitry on the reverse side (bottom) directs electric current to each reservoir. Photographs: left (2) Courtesy of Microchips, Inc./Nature 397, 335-338 (1999). Macmillan Magazines Ltd.;
right (2) Courtesy of Microchips,
Inc./Carita Stubbe When Robert Langer looks out the window of his lab on the edge of the Massachusetts Institute of Technology campus, he sees the future of medicine writ large. To the right sits the Media Lab, a hotbed of silicon-based innovations such as interactive cinema and wearable computers. To the left is MIT Medical, the hub of campus health care.
And here at the crossroads, Langer and his collaborators are working on a device that fuses the best ideas from both institutions.
Langer's team is one of several research groups nationwide developing programmable implants that could revolutionize the way drugs are administered and overcome one of the most common obstacles to effective medical treatment. All too often, getting the right dose of a pharmaceutical to the precise target proves difficult to achieve.
Pills are problematic because the
digestive system breaks down many therapeutic compounds before they
can reach the bloodstream. Injections bypass the stomach but are
expensive and inconvenient, as well as difficult to self-administer.
Worst of all, both needles and pills can cause dangerous
fluctuations of drug concentrations. For example, too much insulin
kills a diabetic; too little can put him in a coma.
Electrical signals pop open the caps, dispersing their contents. Placed beneath the skin near the site of an injury—a sore knee, for instance—one of these smart pills could deliver anti-inflammatory or antiarthritic medication right where it is needed.
Or, implanted directly in a tumor, a microchip could deliver high doses of toxins to the malignant cells without damaging the surrounding organs.
And in the long run, he predicts that the pharmacy chip could even spell the end of today's one-size-fits-all drug treatments. Langer plans to link the programmable chip with sensors and microprocessors that adjust the timing, dosages, and even mixes of medications to a patient's individual needs rather than to societal averages.
The sensors could also function as
24-hour health monitors. Physicians might download a patient's blood
biochemistry readings on demand via a wireless link, evaluate the
response to medication, and adjust the treatment by remote control.
Frequent medical attention could become much cheaper and simpler to
schedule.
The technology will require a host of design refinements before tests on humans can begin, however. In its current form, the pharmacy chip is hardwired to an external battery pack and an unwieldy set of control wires.
He anticipates clinical trials in two to
three years; a finished product could hit the market in 10 years.
The outside of the torpedo is peppered with thousands of microscopic rings composed of an elastic mixture of hydrogel and polymer. Each ring behaves like a biological muscle, contracting when stimulated by an electric current and expanding when the voltage is reversed.
These artificial sphincters do the work of Langer's gold caps in controlling the release of medication, but the rings are far more controllable.
In ChipRx's smart-pill prototype, microscopic rings open and close like sphincters to release medication.
The implant itself is
the size of a matchstick.
His design takes the biological
connection a step further by activating the rings of hydrogel with
biosensors, engineered proteins that bind to target molecules. For
example, an implant for a diabetic would have a biosensor that
reacts to glucose. When a large enough number of glucose molecules
latch onto the biosensor, it would change shape, triggering an
electric current that would shrink the muscles and expose the drug
chambers full of insulin. As glucose levels drop to normal, the
system would shut off.
The device is currently undergoing a basic feasibility test in which it will release its contents into a beaker on command. Although the results are not in yet, pharmaceutical giants such as Bayer and Pharmacia & Upjohn as well as Procter & Gamble have expressed an interest.
And Alison Cole, a program director at the National Institute of General Medical Sciences in Bethesda, Maryland is fairly optimistic.
To begin with, any implant has to contend with the body's natural defenses against foreign intrusions.
Although the company hasn't tested its
camouflage yet, a similar approach has worked well on artificial
heart valves and other devices.
Langer's method is to strive for simplicity, eliminating moving parts in order to minimize the risk of breakdown. Madou is taking an opposite approach, working on backup systems that include a pump to unclog a blocked chamber and a safety valve in case an artificial muscle gets stuck. The ultimate nightmare confronting both inventors is a smart implant that misfires and dispenses a fatal overdose.
One such failure could discredit the
technology and bankrupt its developers.
Kazushi Ishiyama at Tohuku
University in Japan has developed pinhead-sized, magnetically
controlled spinning screws. He envisions smaller versions swimming
through veins, dispensing drugs or burning away cancerous tissue.
It's simply a matter of giving a new twist to the PC revolution, so that patients can benefit from the shotgun marriage going on in Langer's lab.
|