|

by University of
Pittsburgh
September 14, 2020
from
SciTechDaily Website
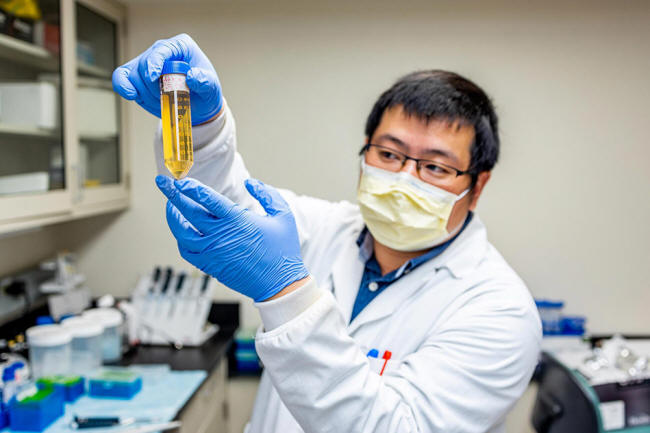
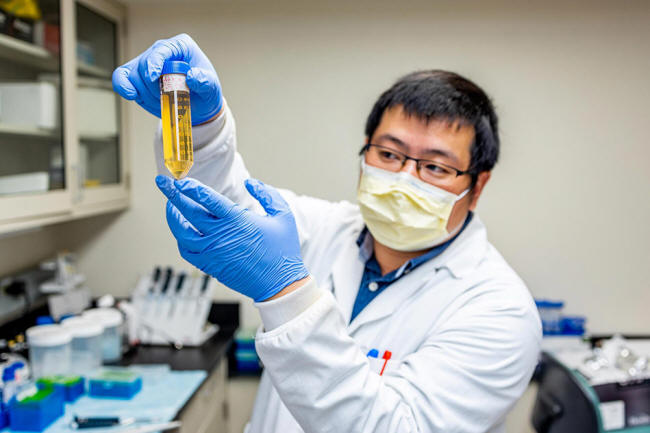
Wei Li, Ph.D., of Pitt,
demonstrates a step in the process
of
obtaining a potential drug
against
COVID-19.
Credit:
UPMC
University of Pittsburgh School of Medicine scientists have isolated
the smallest biological molecule to date that completely and
specifically neutralizes the SARS-CoV-2 virus, which is the cause
of COVID-19.
This antibody component,
which is 10 times smaller than a full-sized antibody, has
been used to construct a drug - known as Ab8 - for potential use as
a therapeutic and prophylactic against SARS-CoV-2.
The researchers report today (September 14, 2020) in the journal
Cell that Ab8 is highly effective in preventing and treating
SARS-CoV-2 infection in mice and hamsters.
Its tiny size not only
increases its potential for diffusion in tissues to better
neutralize the virus, but also makes it possible to administer the
drug by alternative routes, including inhalation.
Importantly, it does not
bind to human cells - a good sign that it won't have negative
side-effects in people.
Ab8 was evaluated in conjunction with scientists from the
University of North Carolina at Chapel Hill (UNC) and
University of Texas Medical Branch (UTMB) at Galveston, as well
as the University of British Columbia and University of
Saskatchewan.
"Ab8 not only has
potential as therapy for COVID-19, but it also could be used to
keep people from getting SARS-CoV-2 infections," said co-author
John Mellors, M.D., chief of the Division of Infectious Diseases
at UPMC and Pitt.
"Antibodies of larger
size have worked against other infectious diseases and have been
well tolerated, giving us hope that it could be an effective
treatment for patients with COVID-19 and for protection of those
who have never had the infection and are not immune."
John Mellors, M.D., chief of infectious diseases,
UPMC and the University of Pittsburgh, discusses a
scientific breakthrough that is a major step toward
a potential drug to treat and prevent COVID-19.
Credit: UPMC
The tiny antibody component is the variable, heavy chain (VH) domain
of an immunoglobulin, which is a type of antibody found in the
blood.
It was found by "fishing" in a pool of more than
100 billion
potential candidates using the SARS-CoV-2 spike protein as bait. Ab8
is created when the VH domain is fused to part of the immunoglobulin
tail region, adding the immune functions of a full-size antibody
without the bulk.
Abound Bio, a newly formed UPMC-backed company, has licensed Ab8 for
worldwide development.
Dimiter Dimitrov, Ph.D.
Credit: University of Pittsburgh
Dimiter Dimitrov, Ph.D., senior author of the Cell publication and
director of Pitt's Center for Antibody Therapeutics, was one of the
first to discover neutralizing antibodies for the original SARS
coronavirus in 2003.
In the ensuing years, his team discovered
potent antibodies against many other infectious diseases, including
those caused by MERS-CoV, dengue,
Hendra and
Nipah viruses.
The
antibody against Hendra and Nipah viruses has been evaluated in
humans and approved for clinical use on a compassionate basis in
Australia.
Clinical trials are testing convalescent plasma - which contains
antibodies from people who already had COVID-19 - as a treatment for
those battling the infection, but there isn't enough plasma for
those who might need it, and it isn't proven to work.
That's why Dimitrov and his team set out to isolate the gene for one
or more antibodies that block the SARS-CoV-2 virus, which would
allow for mass production.
In February, Wei Li, Ph.D., assistant
director of Pitt's Center for Therapeutic Antibodies and co-lead
author of the research, began sifting through large libraries of
antibody components made using human blood samples and found
multiple therapeutic antibody candidates, including Ab8, in record
time.
Then a team at UTMB's Center for Biodefense and Emerging Diseases
and Galveston National Laboratory, led by Chien-Te Kent Tseng,
Ph.D., tested Ab8 using live SARS-CoV-2 virus.
At very low
concentrations, Ab8 completely blocked the virus from entering
cells.
With those results in hand,
Ralph Baric, Ph.D., and his UNC
colleagues tested Ab8 at varying concentrations in mice using a
modified version of SARS-CoV-2.
Even at the lowest dose, Ab8
decreased by 10-fold the amount of infectious virus in those mice
compared to their untreated counterparts.
Ab8 also was effective in
treating and preventing SARS-CoV-2 infection in hamsters, as
evaluated by Darryl Falzarano, Ph.D., and colleagues at the
University of Saskatchewan.
Sriram Subramaniam, Ph.D., and his
colleagues at the University of British Columbia uncovered the
unique way Ab8 neutralizes the virus so effectively by using
sophisticated electron microscopic techniques.
"The COVID-19 pandemic is a global challenge facing humanity, but
biomedical science and human ingenuity are likely to overcome it,"
said Mellors, also Distinguished Professor of Medicine, who holds
the Endowed Chair for Global Elimination of HIV and AIDS at Pitt.
"We hope that the antibodies we have discovered will contribute to
that triumph."
Reference
-
"High potency of a bivalent human VH domain in SARS-CoV-2
animal models" by Wei Li, Alexandra Schäfer, Swarali S. Kulkarni,
Xianglei Liu, David R. Martinez, Chuan Chen, Zehua Sun, Sarah R.
Leist, Aleksandra Drelich, Liyong Zhang, Marcin L. Ura, Alison
Berezuk, Sagar Chittori, Karoline Leopold, Dhiraj Mannar, Shanti S.
Srivastava, Xing Zhu, Eric C. Peterson, Chien-Te Tseng, John W.
Mellors, Darryl Falzarano, Sriram Subramaniam, Ralph S. Baric and
Dimiter S. Dimitrov, Accepted 31 August 2020, Cell.
DOI: 10.1016/j.cell.2020.09.007
-
Additional co-lead authors of this research are Xianglei Liu, M.D.,
Ph.D., of Pitt; Alexandra Schäfer, Ph.D., and David R. Martinez,
Ph.D., both of the University of North Carolina at Chapel Hill; and
Swarali S. Kulkarni, M.Sc., of the University of Saskatchewan.
Additional authors are Chuan Chen, Ph.D., Zehua Sun, Ph.D., Liyoung
Zhang, Ph.D., all of Pitt; Sarah R. Leist, Ph.D., of the University
of North Carolina at Chapel Hill; Aleksandra Drelich, Ph.D., of the
University of Texas Medical Branch; Marcin L. Ura, Ph.D., and Eric
Peterson, M.S., both of Abound Bio; and Alison Berezuk, Ph.D., Sagar
Chittori, Ph.D., Karoline Leopold, Ph.D., Dhiraj Mannar, B.Sc.,
Shanti S. Srivastava, Ph.D., and Xing Zhu, Ph.D., all of the
University of British Columbia.
-
This research was funded by National Institutes of Health grants F32
AI152296, T32 AI007151, AI132178, AI108197 and P30CA016086, as well
as UPMC; the Burroughs Wellcome Fund; a Canada Excellence Research
Chair Award; Genome BC, Canada; Canadian Institutes for Health
Research; and Canadian Foundation for Innovation.
|