|
from
TheGuardian Website
since the first 'test-tube baby', how close are we to editing out all of our genetic imperfections, and should we even try to do so?
Each embryo has a description, something like this:
There are 200 of these embryos to choose from, all made by in vitro fertilization (IVF) from you and your partner's eggs and sperm.
So, over to you. Which
will you choose...?
Inspired by predictions
about the future of reproductive technology by the biologists
J.B.S. Haldane and Julian Huxley in the 1920s, Huxley's
brother Aldous wrote a satirical novel about it.
Set in the year 2540, it describes a society whose population is grown in vats in an impersonal central hatchery, graded into five tiers of different intelligence by chemical treatment of the embryos. There are no parents as such - families are considered obscene.
Instead, the gestating fetuses and babies are tended by workers in white overalls,
Brave New World has become the inevitable reference point for all media discussion of new advances in reproductive technology.
Whether it's Newsweek reporting in 1978 on the birth of Louise Brown, the first "test-tube baby" (the inaccurate phrase speaks volumes) as a,
...the message is that we are heading towards Huxley's hatchery with its racks of tailor-made babies in their "numbered test tubes".
The spectre of a harsh, impersonal and authoritarian dystopia always looms in these discussions of reproductive control and selection.
Novelist Kazuo Ishiguro, whose 2005 novel, Never Let Me Go, described children produced and reared as organ donors, last month warned that thanks to advances in gene editing,
But the prospect of genetic portraits of IVF embryos paints a rather different picture.
If it happens at all, the aim will be not to engineer societies but to attract consumers.
I don't think we are going to see superman or a split in the species any time soon,
because we just don't know enough. bioethicist
Ishiguro's dire forecast was spurred by the gene-editing method called Crispr-Cas9, developed in 2012, which uses natural enzymes to target and snip genes with pinpoint accuracy.
Thanks to Crispr-Cas9, it seems likely that gene therapies - eliminating mutant genes that cause some severe, mostly very rare diseases - might finally bear fruit, if they can be shown to be safe for human use.
Clinical trials are now
under way.
And Kathy Niakan
of the
Francis Crick Institute in the UK
has been granted a licence by the Human Fertilization and
Embryology Authority (HFEA)
to use Crispr-Cas9 on embryos a few days old to find out more about
problems in these early stages of development that can lead to
miscarriage and other reproductive problems.
A team of scientists warned in Nature less than two years ago that genetic manipulation of the germ line (sperm and egg cells) by methods like Crispr-Cas9, even if focused initially on improving health,
Besides, there seems to be little need for gene editing in reproduction.
It would be a difficult, expensive and uncertain way to achieve what can mostly be achieved already in other ways, particularly by just selecting an embryo that has or lacks the gene in question.
Because of unknown health risks and widespread public distrust of gene editing, bioethicist Ronald Green of Dartmouth College in New Hampshire says he does not foresee widespread use of Crispr-Cas9 in the next two decades, even for the prevention of genetic disease, let alone for designer babies.
However, Green does see gene editing appearing on the menu eventually, and perhaps not just for medical therapies.
He warns that this might be accompanied by,
For now, though, if there's going to be anything even vaguely resembling the popular designer-baby fantasy, Henry Greely says it will come from embryo selection, not genetic manipulation.
Embryos produced by IVF will be genetically screened - parts or all of their DNA will be read to deduce which gene variants they carry - and the prospective parents will be able to choose which embryos to implant in the hope of achieving a pregnancy.
Greely foresees that new
methods of harvesting or producing human eggs, along with advances
in preimplantation genetic diagnosis (PGD)
of IVF embryos, will make selection much more viable and appealing,
and thus more common, in 20 years' time.
The testing, generally on three- to five-day-old embryos, is conducted in around 5% of IVF cycles in the US.
In the UK it is performed
under licence from the
HFEA, which permits screening for
around 250 diseases including thalassemia, early-onset Alzheimer's
and cystic fibrosis.
But that will change, he says, thanks to developments that will make human eggs much more abundant and conveniently available, coupled to the possibility of screening their genomes quickly and cheaply.
Carey Mulligan, Keira Knightley and Andrew Garfield in the 2010 film adaptation of Kazuo Ishiguro's 'Never Let Me Go,' in which clones are produced to provide spare organs for their originals.
Photograph: 20th Century Fox/Everett/Rex
But using genetic data to predict what kind of person an embryo would become is far more complicated than is often implied.
Seeking to justify unquestionably important research on the genetic basis of human health, researchers haven't done much to dispel simplistic ideas about how genes make us.
Talk of,
...has led to a widespread perception that there is a straightforward one-to-one relationship between our genes and our traits.
In general, it's anything
but...
Most more common diseases
or medical predispositions - for example, diabetes, heart disease or
certain types of cancer - are linked to several or even many genes,
can't be predicted with any certainty, and depend also on
environmental factors such as diet.
Even if they are strongly
inheritable - it's estimated that up to 80% of intelligence, as
measured by IQ, is inherited - we don't know much at all about which
genes are involved, and not for want of looking.
That's not much use.
Even these,
...but as the number of
people whose genomes have been sequenced increases, the predictive
ability will improve substantially.
But that information,
If the genetic basis of attributes like intelligence and musicality is too thinly spread and unclear to make selection practical, then tweaking by genetic manipulation certainly seems off the menu too.
If this is all "designer
babies" could mean even in principle - freedom from some specific
but rare diseases, knowledge of rather trivial aspects of
appearance, but only vague, probabilistic information about more
general traits like health, attractiveness and intelligence - will
people go for it in large enough numbers to sustain an industry?
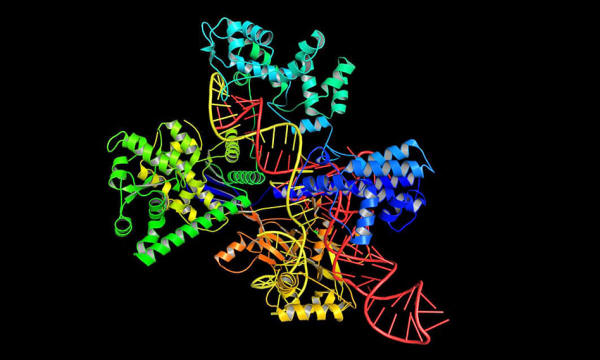
uses a molecular structure to edit genomes.
Photograph: Alamy
In the next 40-50 years, he says,
He's less optimistic about the consequences, saying that we will then see social tensions,
As Greely points out, a
perfectly feasible 10-20% improvement in health via PGD, added to
the comparable advantage that wealth already brings, could lead to a
widening of the health gap between rich and poor, both within a
society and between nations.
The poor take-up of sperm banks offering "superior" sperm, she says, already shows that.
For most women,
R. Alta Charo feels that,
All the same, societies are going to face tough choices about how to regulate an industry that offers PGD with an ever-widening scope.
One of the easiest things to screen for is sex.
Gender-specific abortion is formally forbidden in most countries, although it still happens in places such as China and India where there has been a strong cultural preference for boys.
But prohibiting selection by gender is another matter.
Once selection beyond avoidance of genetic disease becomes an option - and it does seem likely - the ethical and legal aspects are a minefield.
She adds:
A scientist at work during an IVF process. Photograph: Ben Birchall/PA
The production of embryos for IVF must become easier, more abundant and less unpleasant. And gene sequencing must be fast and cheap enough to reveal the traits an embryo will have.
Put them together and you have "Easy PGD" (preimplantation genetic diagnosis):
One possibility is a one-off medical intervention that extracts a slice of a woman's ovary and freezes it for future ripening and harvesting of eggs.
It sounds drastic, but
would not be much worse than current egg-extraction and
embryo-implantation methods. And it could give access to thousands
of eggs for future use.
Last October (2016), a
team in Japan reported that they had made mouse eggs this way from
skin cells, and fertilized them to create apparently healthy and
fertile mouse pups.
In 2009 it cost around $50,000. Today it is most like $1,500, which is why several private companies can now offer this service. In a few decades it could cost just a few dollars per genome.
Then it becomes feasible to think of PGD for hundreds of embryos at a time.
He thinks it will then become common for children to be conceived through IVF using selected genomes.
He forecasts that this will lead to,
|