|
by Dr. Joseph Mercola
November 17, 2024
from
Mercola Website
PDF Version

Unlock the Gut Health
Secret Doctors don't Discuss
- Your Immune System's hidden
Ally Revealed.
Discover how an imbalanced microbiome
silently erodes immunity and
overall wellness,
leading to chronic health
issues that may surprise you.
Learn practical steps to
strengthen your body's
natural defenses, optimize gut
health, and transform
your energy and resilience with
expert-backed insights
that go beyond probiotics.
Story at-a-glance
-
Your
microbiome plays an important role in training your
immune system, with gut dysfunction and increased
permeability often leading to autoimmune diseases and
inflammation
-
A
healthy colon requires an oxygen-free environment for
beneficial bacteria, but environmental toxins and
compromised mitochondrial function disrupt this delicate
balance
-
Modern environmental toxins, including microplastics and
EMFs, act as mitochondrial poisons, increasing oxygen in
the colon and promoting growth of harmful bacteria
-
Health coaching is a key component of sustainable
wellness, providing necessary support and accountability
while helping patients implement lasting lifestyle
changes
Understanding the intricate connections between your immune system,
gut health and overall well-being is a key part of reaching optimal
health.
Recently, I had the privilege of interviewing Dr.
Heather Moday, founder of The Moday Center based in
Virginia, who has seamlessly integrated functional and integrative
medicine into her practice.
Our conversation focused on significant shifts in medical practice,
the critical role of
the microbiome and the
indispensable value of health coaching in achieving lasting health
outcomes.
A Journey from Conventional to
Integrative Medicine
Dr. Moday's medical journey is a testament to the profound impact
that integrative and functional medicine have on patient care.
Beginning her career with a solid foundation in
internal medicine, she pursued a fellowship in allergy and
immunology, spending a decade in private practice addressing
allergies, chronic asthma and immune deficiencies.
"I felt that I wasn't using really all that I
had learned, and there was a lot more to learn. It was not
holistic enough for me," Moday shared. 1
This sentiment drove her to search for a more
comprehensive understanding of health via an integrative medicine
fellowship with Dr. Andrew Weil in Arizona and subsequent
certification in functional medicine in 2014.
This pivotal transition allowed Moday to expand her focus,
beyond
conventional immunology, embracing a holistic framework that
considers nutrition, behavior and environmental factors as
components of health.
By bridging these disciplines, she now addresses
chronic medical issues with a more nuanced and effective approach.
Your Microbiome Is the Heartbeat
of Your Immune System
The microbiome - the vast ecosystem of microbes residing primarily
in your colon - was a primary focus of our discussion.
Moday explained how these trillions of
microorganisms are not merely passive inhabitants but active
participants in training your immune system and maintaining overall
health.
"[The microbiome] literally trains our immune
system, but it also informs and acts as a go-between," she said.
2
These microbes foster a balanced immune response,
preventing conditions like chronic inflammation, autoimmune
disorders and metabolic diseases such as diabetes and obesity.
We also discussed leaky gut, a condition where
the epithelial lining of your digestive tract becomes permeable.
This increased permeability allows unwanted substances like
endotoxins (lipopolysaccharides, or LPS) and food antigens to enter
your bloodstream, triggering immune responses that lead to
autoimmune diseases.
In fact, in most cases you cannot have an
autoimmune disease unless you have some type of gut dysfunction.
Maintaining the integrity of your gut barrier
is paramount, but
factors such as stress, poor nutrition, environmental toxins and
certain medications often compromise this barrier, leading to,
systemic inflammation and immune dysregulation...
Your Gut's
Hidden Heroes Will Help You Reclaim Your Vitality
Your colon maintains a controlled oxygen gradient that is crucial
for the growth of oxygen-intolerant bacteria.
It's like having different climate zones within
your gut, each supporting specific types of bacterial life. This
gradient isn't static; it requires a constant supply of cellular
energy to maintain.
If that energy supply falters, oxygen can seep in, killing off your
beneficial bacteria.
As beneficial bacteria dwindle in numbers, more
harmful, oxygen-tolerant species gain ground. This imbalance then
sets the stage for a range of other health issues.
Maintaining this oxygen gradient is one of the most important, yet
often overlooked, aspects of gut health. It's not just about what
you eat, but about creating the right environment for your
beneficial bacteria to thrive.
This is where the importance of cellular energy
production comes into play.
Without it, the entire system can collapse.
And what do we have to thank for maintaining
this system?
Some of the hardest-working cells in your body:
colonocytes and goblet cells.
Colonocytes line your colon walls, performing
many vital functions.
They're like the bouncers at an exclusive
club, deciding what gets in and what stays out. They also play a
crucial role in maintaining that all-important oxygen gradient.
Goblet cells, on the other hand, are the maintenance crew.
They secrete a mucus that acts as a
protective coating, shielding your gut lining from harmful
substances and pathogens.
Colonocytes and goblet cells form a strong
defense for your gut.
The health of these cells is directly linked to
your overall gut health and, by extension, your general well-being.
When they work well, they help build a strong gut barrier, absorb
nutrients, and balance the microbiome.
But when compromised, it can lead to many
digestive and systemic health issues.
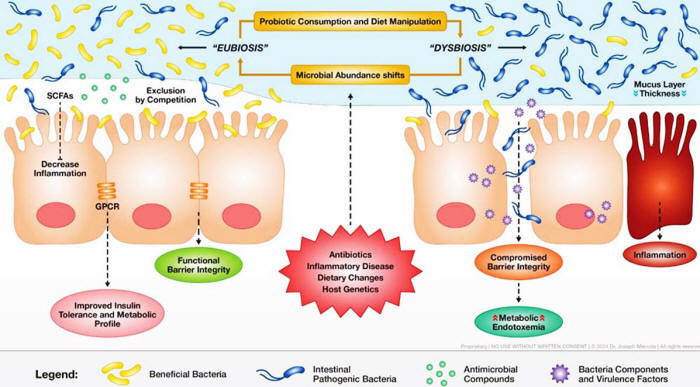
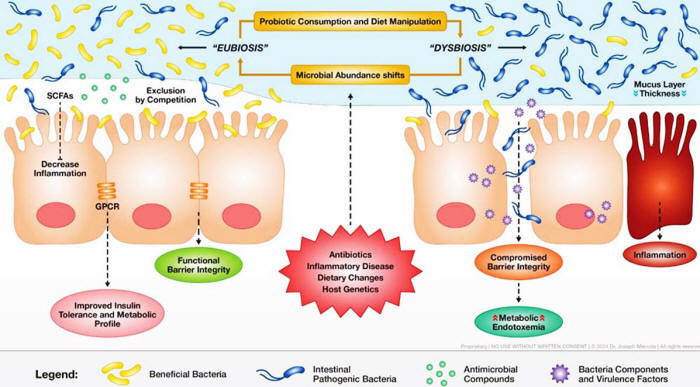
This illustration depicts the delicate balance of gut microbiota and
its impact on health.
On the left, "Eubiosis" shows a healthy gut
environment with beneficial bacteria, strong barrier integrity,
and positive metabolic outcomes.
On the right, "Dysbiosis" demonstrates how
factors like antibiotics and an inappropriate diet can disrupt
this balance, leading to inflammation and compromised gut
health.
Probiotic consumption and diet can cause dramatic
shifts in microbial abundance, influencing everything from
mucus-layer thickness to insulin tolerance and metabolic profile.
Mitochondrial Function and Its
Role in Gut Health
Mitochondria, often referred to as the powerhouses of the cell, are
integral to energy production.
In your colon, colonocytes - the epithelial
cells lining your colon - rely heavily on mitochondrial energy
to perform fatty acid oxidation.
Interestingly, mitochondria themselves are
believed to have originated from primordial bacteria through an
evolutionary process known as endosymbiosis.
While mitochondria are present in colonocytes,
bacteria within your gut microbiome do not possess mitochondria and
instead survive on glycolysis.
This symbiotic relationship underscores the
intricate connections between your cellular biology and microbial
inhabitants.
However, despite your colon's naturally low-oxygen environment,
modern-day exposure to environmental toxins threatens to disrupt
this balance.
We're all exposed to a soup of environmental
toxins, including,
microplastics, vegetable oils rich in
linoleic
acid and
electromagnetic fields (EMFs)...
These toxins act as mitochondrial poisons,
impairing the energy production necessary for maintaining your
colon's oxygen-free state.
When mitochondria are compromised, colonocytes cannot effectively
consume the limited oxygen, leading to an increase in oxygen within
your colon.
This shift creates an environment conducive to
the growth of facultative anaerobes - oxygen-tolerant bacteria that
are often pathogenic.
When your mitochondria don't have enough energy, the colonocytes
tend to not thrive, and the oxygen in your colon progressively
increases.
This leads to a decrease in beneficial
bacteria and their replacement by pathogenic bacteria.
Endotoxins, specifically LPS, are another factor
in this equation, and there's a significant difference between
endotoxins produced by obligate anaerobes and those from facultative
anaerobes.
The endotoxin from obligate anaerobes is much
less pernicious and doesn't kill you prematurely, but the
facultative ones do.
Pathogenic facultative anaerobes produce more harmful LPS, which
triggers chronic inflammation and contributes to various health
disorders, including autoimmune diseases and metabolic syndrome.
Challenges in Recolonizing Your
Gut with Beneficial Bacteria
Replenishing your gut with beneficial bacteria like Akkermansia
presents significant challenges, as there is virtually no company
that produces an Akkermansia product that reaches the colon
effectively.
The primary obstacle lies in the fragility of these bacteria:
they are highly sensitive to oxygen and
require specialized protective capsules to survive the journey
through the digestive tract.
Currently available supplements often fail to
deliver live bacteria to the colon, rendering them ineffective for
recolonization purposes.
I'm actively funding research to identify and cultivate new species
of obligate anaerobes that produce beneficial metabolites in the
microbiome.
We've identified dozens of species that are most
likely, based on genomic analysis, to produce beneficial metabolites
in the microbiome.
This ongoing research holds promise for expanding
the repertoire of effective probiotics that support a healthy gut
environment.
Insulin Resistance, Oxidative
Stress and Metabolic Health
Insulin resistance is a widespread issue, often serving as a
precursor to more severe metabolic conditions.
During our discussion, I introduced the
Homeostatic Model Assessment of Insulin Resistance (HOMA-IR), a
simple yet highly effective tool for assessing insulin sensitivity.
HOMA-IR involves measuring fasting blood glucose and insulin levels
to provide a reliable indicator of insulin resistance.
This method is both cost-effective and
accessible, making it a valuable tool for early detection and
intervention. Moday concurred, acknowledging its utility in her
practice and emphasizing that most individuals exhibit some degree
of insulin resistance.
Oxidative stress, driven by an imbalance between free radicals and
antioxidants, is another factor in cellular damage and disease
progression.
Our conversation highlighted the nuanced
relationship between oxidative and reductive stress, particularly in
the context of mitochondrial health.
Free radicals, such as superoxide and hydroxyl radicals, are highly
reactive molecules that damage cellular components.
Antioxidants neutralize these free radicals,
preventing oxidative stress.
However, I emphasized that in many
cases, free radicals are generated from
reductive stress, where an
excess of electrons leads to the formation of harmful reactive
oxygen species (ROS).
Addressing environmental toxin exposure is a multifaceted endeavor.
Moday recommended simple, actionable steps such
as,
-
avoiding plastic containers
-
opting for stainless steel or glass
alternatives
-
minimizing the use of processed foods laden with
additives and preservatives...
"You can start with something as simple as
not drinking your coffee out of a traditional plastic Styrofoam
cup... you can buy a very cheap stainless steel coffee mug and
water bottle, and you can drink out of those," she advised.
3
These small changes, when implemented
consistently, significantly reduce your body's toxin burden and
support overall health.
Health Coaching Provides an
Essential Support System for Lasting Change
We also discussed the role of health coaching in facilitating
sustainable health improvements.
Moday shared her experiences and underscored the
importance of personalized support in achieving behavioral and
lifestyle changes.
While proper health care and nutritional guidance are vital, without
addressing sleep, stress, and overall lifestyle, patients often
struggle to achieve meaningful results.
Health coaches provide the necessary support,
accountability and personalized strategies to help individuals
navigate these changes effectively.
Moday believes health coaching should be integrated into a
comprehensive health care approach.
By collaborating with health coaches, patients
receive a holistic support system that addresses both physical and
emotional aspects of health. This collaborative model enhances
patient outcomes and fosters long-term well-being.
We're developing an innovative solution to address this very
challenge - the Mercola Health Coach app, scheduled for
launch this November.
Like Dr. Mode, we recognize the critical need for
practical support in implementing life-changing health practices.
This revolutionary tool will provide the guidance and support needed
to help people successfully adopt important biological optimization
strategies that often feel overwhelming or complex.
Our goal is to make these vital health
transformations more accessible and achievable for everyone.
If you're interested and being put on the wait
list for this app you can
click this link.
The Epidemic of Allergies -
Lessons from Peanut Allergy Trends
Our interview also touched on the alarming rise in food allergies,
particularly peanut allergies, and the factors contributing to this
trend.
The hygiene hypothesis suggests that reduced
exposure to microbes in early childhood leads to an underdeveloped
immune system, increasing susceptibility to allergies and autoimmune
diseases.
Moday expanded on this by introducing the "Good Friends Hypothesis,"
which emphasizes the importance of maintaining a diverse and
beneficial microbiome through appropriate microbial exposure...
"In the ‘90s, someone came up with the idea
that children should not be introduced to peanut antigens until
they were 3 or 4 years old.
But that was problematic," she said.
4
By not exposing children to these allergens
during critical developmental periods, we inadvertently heightened
their immune sensitivity.
Current research supports early introduction as a
strategy to promote immune tolerance and reduce the risk of
allergies.
A Holistic Path
to Health
My interview with Moday reaffirmed,
the profound interconnectedness
of our immune system, gut health and overall well-being.
By embracing integrative and functional medicine,
addressing environmental toxins and incorporating health coaching,
we can overcome modern health challenges with greater efficacy and
compassion.
The journey to optimal health is multifaceted and requires a
commitment to continuous learning and adaptation.
As we advance, the collaboration between medical
professionals, researchers and health coaches will be key in
fostering a health care system that prioritizes holistic,
patient-centered care.
Together, by implementing these insights and strategies, we'll
unlock the full potential of our bodies, enhance our resilience
against chronic diseases and achieve a higher state of well-being.
To learn more about Moday and her integrative
approach to medicine, follow her on Instagram at
@doctormoday.
Video
Interview transcript
Sources and References
-
Youtube, Dr. Mercola, Revealing Links Between Gut
Health, Immunity and Wellness - Interview with Dr.
Heather Moday, 1:03
-
Youtube, Dr. Mercola, Revealing Links Between Gut
Health, Immunity and Wellness - Interview with Dr.
Heather Moday, 6:40
-
Youtube, Dr. Mercola, Revealing Links Between Gut
Health, Immunity and Wellness - Interview with Dr.
Heather Moday, 42:12
-
Youtube, Dr. Mercola, Revealing Links Between Gut
Health, Immunity and Wellness - Interview with Dr.
Heather Moday, 37:03
|