Editor’s Note
This compelling article by Dr. Kelly Brogan
is sure to get you thinking about gluten and whether it could be
contributing in a massive way to the skyrocketing cases of
autoimmune illness today.
If you would like to learn more,
consider free registration for the
Gluten Summit
hosted by Dr. Tom O’Bryan, the world’s leading gluten expert,
which kicks off Monday, November 11, 2013.
Learn more here.

“You should consider eliminating all gluten and dairy from your
diet for 3 months.”
Gulp.
Those words hung in the air like an alien spacecraft hovering
between us.
When I had the good sense to consult a naturopath after my
diagnosis with postpartum thyroiditis, this was the backbone of
her recommendation to me. To me, as a psychiatric fellow, 9
years into my medical training, gluten had no relevance to the
non-celiac population.
Celiac disease was a rare and
unfortunate affliction that made living a “normal” life
impossible because of the strict prohibition on, what seemed to
me at the time, all food. Raised on classic Italian pastas,
lasagnas, and paninis, and a NYC pizza and bagel-ophile, I
honestly couldn’t conceive of what I would eat.
Fast-forward
five years, several hundred medical journal articles,
conferences, seminars, and a personal health revolution later,
and I am now convinced of the imperative for all people to
eliminate this inflammatory food from their lives.
I plan to
detail - be forewarned: science to follow - the information that
made me change my tune on this seemingly innocuous, but quite
ubiquitous “food”.
Here’s the goods in 1500 words:
We Know Why and How it Hurts You
Sometimes, as I read a medical paper, I get this euphoric
rush that makes time seem to slow down (nerd alert).
I grip the
pages a bit tighter and I savor what is to come because I know
that I am experiencing paradigm-shifting information, first
hand. When I read
this paper by
Alessio Fasano in 2011, I knew the processed food industry
was going to have to think fast to get out from under this
knowledge.
In a feat of scientific brilliance, he connected the
dots for us and explained the following:
-
The gut does more than absorb food
- it is the barrier determinant of self and non-self that
educates the immune system. Here is where our bodies learn
about what to attack, and where they can be miseducated
about attacking themselves (autoimmunity).
-
The trafficking of macromolecules across the gut barrier
requires a facilitator - a doorman who lets them through.
This agent is called zonulin and opens the spaces or tight
junctions between gut cells.
-
Zonulin is triggered by gliadin which is the protein
found in the grains wheat, rye, and barley. This triggering
occurs in 80% of the population based on hereditary
haplotypes.
-
There is reason to suspect that prolamine grains
including the above and corn, sorghum, and oats (called this
because of their high proline and glutamine content) may all
play a role in triggering these dynamic gut changes.
Cross-reactivity and stimulation of alpha gliadin by foods
like dairy, oats, corn, millet, and even instant coffee was
examined in
this study suggesting that those with limited clinical
improvement on a gluten free diet (but with positive
antibodies) should also consider broader eliminations.
-
Immune activation is mediated by
changes in gut permeability and blood brain permeability.
Essentially, once local inflammation is kicked off and the
door to the blood stream is opened, the immune system
responds. This permeability also allows for the passage of
toxins from bacteria called lipopolysaccharide that may play
a significant role in depression as discussed
here.
Inflammation
and Immune Stimulation
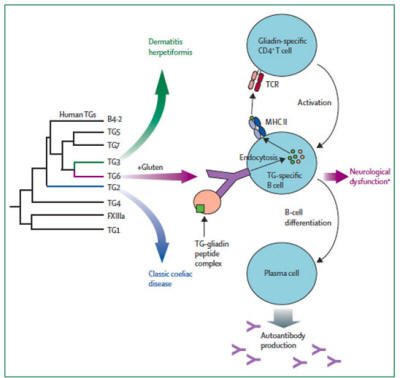
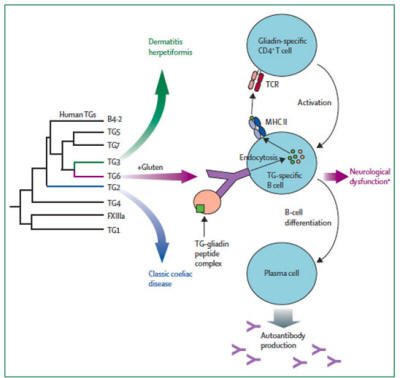
The nature of this immune response is becoming better
elucidated. Here are some important conceptual players:
Molecular Mimicry
This is an immunologic concept that appears to lie at the
root of a lot of what ails us in this world full of foreign
particles.
The immune system reacts to unknown/novel compounds
through the innate system, which is mediated by white blood
cells including macrophages and dendritic cells, complement
cascades, natural killer cells, and cytokines.
This arm of the
immune system instructs the “learned” or adaptive system, which
employs B cells and T cells to build antibodies that continues
to re-recognize the offending agent.
Once gliadin peptides in gluten have breached the gut mucosa,
they can stimulate production of an array of antibodies and
other tissue impairing agents:
-
Alpha/beta, gamma, and omega gliadin
antibodies
-
Endomesial tissue antibodies
-
Tissue transglutaminase: Tissue transglutaminase is an
enzyme that plays an important role in presenting gliadin to
B and T cells to be marked for antibody production.
This
enzyme is tagged as part of the complex with gluten and
becomes a target of the immune system. Importantly, transglutaminase 6 is active in the central nervous system
and appears to mediate the neurologic effects of gluten
intolerance including,
...as discussed
here
and
here.
Importantly, transglutaminase deposits accumulate
in blood vessels including the blood brain barrier.
-
Synapsin, GAD (glutamic acid decarboxylase), and
gangliodise: 51% of the Celiac population develops
neurologic or psychiatric dysfunction, and significant
percentages of neurologic diseases such as ataxia, seizures,
and neuropathy are found to be driven by and resolved by
gluten exposure as discussed
here.
One study found that 27% of schizophrenics had gliadin
antibodies. Once again, molecular mimicry is at the
foundation of gliadin-reactive antibodies that target
cellular components of the nervous system influencing
neurochemical transmission.
Neurological manifestations most
often present in the absence of any report of
gastrointestinal symptoms.
-
Thyroid auto-antibodies: Autoimmune
thyroid disease occurs in unexpected frequency in Celiac
patients leading researchers to identified shared pathology
to these two conditions.
Molecular mimicry and amino acid
motif overlap in gliadin and the thyroid enzyme peroxidase
and protein thyroglobulin may trigger cross-reactivity in
the setting of intestinal permeability and immune response
to gluten. Tissue transglutaminase antibodies also bind
thyroid tissue causing gland destruction and recruitment of
the immune system for repair.
The inflammatory cytokine
IL-15 is a shared mechanism for immune reactivity in Celiac
disease and Hashimoto’s thyroiditis thought to drive
inflammation that is furthered by poor selenium absorption
when the gut lining is compromised (as discussed
here).
Selenium is not only integral for thyroid hormone function,
but is also an antioxidant that does damage control in the
setting of oxidative stress.
Gluten is a Drug
Independent of the brain effects already discussed, gliadin
peptides may travel through the blood stream can stimulate
opiate receptors in the brain resulting in their being termed
gliadorphins.
The effects of this stimulation may have
wide-ranging psychiatric manifestations, not the least of which
is the addictive potential of these foods. Those eating high
gluten diets can expect to undergo 1-3 weeks of withdrawal
symptoms upon cessation.
This type of a relationship with a food
raises flags for this psychiatrist!
Leak-inducing Lectins
You may have sprinkled wheat germ on your cereal for a little
health boost or even been recommended sprouted grain bread as a
wellness intervention sanctioned by gurus everywhere.
These
foods contain the highest and best-studied levels of lectin, an
anti-nutrient and partner in crime to gliadin peptides in wheat,
barley, and rye, but present in many foods and most in grains,
legumes, and dairy (and notably genetically modified foods
designed to increase lectin content for pest control).
They are
the plant world’s natural defense, the thorn on the rose meant
to inspire regret in those who deign to feast on them. Lectins
promote intestinal inflammation and permeability, and then cause
wide-spread and varied organ damage by binding with sugars in
body tissues.
Lectins can be minimized but not eliminated by
processing/preparation of grains and beans, and is one of the
reasons white rice is recommended over brown.
GMO Guts Primed for Gluten-related Damage
One of the primary reasons that I, and many educated others,
believe that genetically modified foods are the death by one
thousand cuts of modern man is because of their impact on the
gut.
Bt-toxin and glyphosate are two poisons heavily employed in
the production of genetically modified crops. Bt-toxin is used
in corn as a “natural” pesticide the American public has been
assured does not affect the human body.
Its perforating effects
on insect digestive tracts does not appear to be limited to
these pests, as this toxin has been
found
in fetal circulation (implying that it obviously violated the
gut barrier of pregnant women consuming these products).
Herbicides such as the heavily
employed RoundUp, have now been
revealed
to have active bacteria-killing and inflammatory effects in our
guts, changing our microbiome with every dose we consume.
Vegetable oils, soy, corn, and animals consuming corn are a
ubiquitous part of the modern diet that likely perpetuates gut
dysfunction that then facilitates the immune-based effects of
gluten exposure.
Testing
The limitations of currently available conventional testing
are very real as most physicians who do a “Celiac panel” are
only testing for alpha gliadin, tissue transglutaminase 2, and
endomesial antibody.
As discussed above, in a grain consisting
of 6 sets of chromosomes, capable of producing greater than
20,000 proteins, this testing may just be too small a window
into a very complex space.
You, Me, Us
Some degree of gluten reactivity is thought to occur in up to
80% of the population and is driven by shared and distinct
immune response mechanisms.
Response to gluten free diets in
placebo-controlled trials and inflammation in the guts of
non-Celiac patients, even without gliadin antibodies (such as in
this study of exposed non-Celiac patients) argues for the
universal effects of this food, and the individuality of our
immune responses accounting the variations in severity and
presentation.
This paper (The
Dietary Intake of Wheat and other Cereal Grains and Their Role
in Inflammation) is an incredible review and is named on my
desktop, “The Mother of all Gluten Papers”, if you’d like to
delve into the topic and references.
Celiac
incidence has increased more than 4 fold in the past 50
years which may be attributable to the increased gluten content
of wheat secondary to hybridization techniques, increased
consumption, combined exposure to a number of environmental
toxins, and associated microbiome changes.
As Sayer Ji of GreenMedInfo.com discusses
here, it is possible that
Celiac Disease is an adaptive,
symptom-producing response to an environmental toxin we, as a
species are not meant to consume. The rest of us are having
vague, cumulative malaise and immune-mediated effects that we
have more difficulty associating to the source - consuming
grains.
I’m here to help expedite your healing.
Stop . Eating . Gluten . Now
There are many
wonderful and freely available
guides to converting to a gluten free life, but the basic
principle is to eliminate rye, barley, wheat, and unspecified
oats.
The difficulty is in identifying the hidden sources of
gluten in sauces, condiments, soups, and flavorings.
Essentially, going gluten-free should mean eliminating processed
food from your life, which is why I have a low threshold to also
recommend elimination of co-reactive foods like dairy (casein),
corn, soy, and in some cases legumes (including peanuts), and
gluten free grains like rice and millet.
After gut healing,
quinoa, amaranth, and buckwheat may be less stimulatory as they
are technically dicots and may not overlap as much with monocot
grains. For emergencies, the enzyme DPPIV is available over the
counter and
may help
aid in the digestion of gluten grains with “accidental”
exposure.
Here is a great
guide to pesticide free shopping, and a
guide to
avoiding
genetically modified foods.
Armed with this information, I’m hoping that those suffering
from neurologic, psychiatric, gastrointestinal, or otherwise
undiagnosable health concerns might consider this palliative
intervention.
It may be the last prescription you’ll ever need.