|

by Anne Trafton
February
20, 2020
from
NewsMIT Website
Italian version
MIT researchers
used a machine-learning algorithm
to identify a drug called halicin that
kills many strains of bacteria.
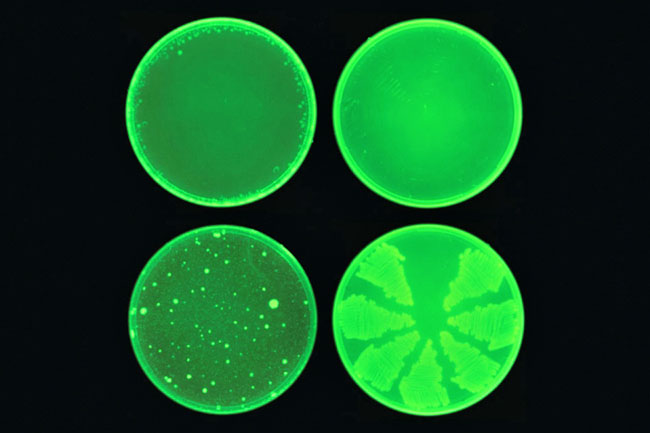
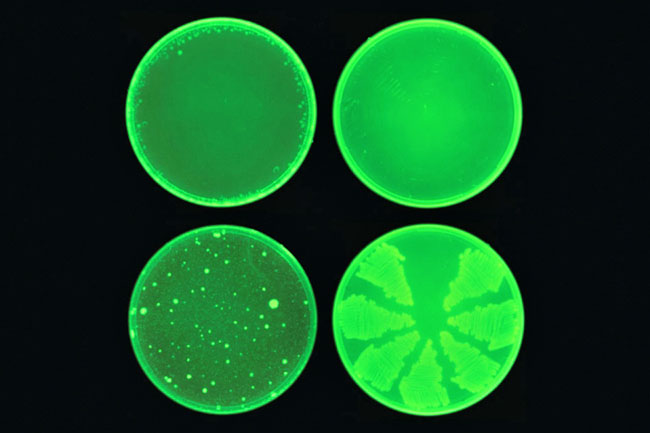
Halicin (top row) prevented the development of
antibiotic resistance in E. coli,
while ciprofloxacin (bottom row) did not.
Image: courtesy of the Collins Lab at MIT
A
deep-learning model
identifies a
powerful new drug
that can kill
many species
of
antibiotic-resistant bacteria...
Using a machine-learning algorithm, MIT researchers have identified
a powerful new antibiotic compound.
In laboratory tests, the
drug killed many of the world's most problematic disease-causing
bacteria, including some strains that are resistant to all known
antibiotics. It also cleared infections in two different mouse
models.
The computer model, which can screen more than a hundred million
chemical compounds in a matter of days, is designed to pick out
potential antibiotics that kill bacteria using different mechanisms
than those of existing drugs.
"We wanted to develop
a platform that would allow us to harness the power of
artificial intelligence to usher in a new age of antibiotic drug
discovery," says James Collins, the Termeer Professor of Medical
Engineering and Science in MIT's Institute for Medical
Engineering and Science (IMES) and Department of Biological
Engineering.
"Our approach
revealed this amazing molecule which is arguably one of the more
powerful antibiotics that has been discovered."
In their new study, the
researchers also identified several other promising antibiotic
candidates, which they plan to test further.
They believe the model
could also be used to design new drugs, based on what it has learned
about chemical structures that enable drugs to kill bacteria.
"The machine learning
model can explore, in silico, large chemical spaces that can be
prohibitively expensive for traditional experimental
approaches," says Regina Barzilay, the Delta Electronics
Professor of Electrical Engineering and Computer Science in
MIT's Computer Science and Artificial Intelligence Laboratory (CSAIL).
Barzilay and Collins, who
are faculty co-leads for MIT's Abdul Latif Jameel Clinic for Machine
Learning in Health (J-Clinic), are the senior authors of the study
(A
Deep Learning Approach to Antibiotic Discovery),
which appears today in Cell.
The first author of the
paper is Jonathan Stokes, a postdoc at MIT and the Broad
Institute of MIT and Harvard.
A new pipeline
Over the past few decades, very few new antibiotics have been
developed, and most of those newly approved antibiotics are slightly
different variants of existing drugs.
Current methods for
screening new antibiotics are often prohibitively costly, require a
significant time investment, and are usually limited to a narrow
spectrum of chemical diversity.
"We're facing a
growing crisis around antibiotic resistance, and this situation
is being generated by both an increasing number of pathogens
becoming resistant to existing antibiotics, and an anemic
pipeline in the biotech and pharmaceutical industries for new
antibiotics," Collins says.
To try to find completely
novel compounds, he teamed up with,
...who have previously
developed machine-learning computer models that can be trained to
analyze the molecular structures of compounds and correlate them
with particular traits, such as the ability to kill bacteria.
The idea of using predictive computer models for "in silico"
screening is not new, but until now, these models were not
sufficiently accurate to transform drug discovery.
Previously, molecules
were represented as vectors reflecting the presence or absence of
certain chemical groups.
However, the new neural
networks can learn these representations automatically, mapping
molecules into continuous vectors which are subsequently used to
predict their properties.
In this case, the researchers designed their model to look for
chemical features that make molecules effective at killing E. coli.
To do so, they trained
the model on about 2,500 molecules, including about 1,700
FDA-approved drugs and a set of 800 natural products with diverse
structures and a wide range of bioactivities.
Once the model was trained, the researchers tested it on the Broad
Institute's Drug Repurposing Hub, a library of about 6,000
compounds. The model picked out one molecule that was predicted to
have strong antibacterial activity and had a chemical structure
different from any existing antibiotics.
Using a different
machine-learning model, the researchers also showed that this
molecule would likely have low toxicity to human cells.
This molecule, which the researchers decided to call
halicin, after
the fictional artificial intelligence system from "2001: A Space
Odyssey," has been previously investigated as possible diabetes
drug.
The researchers tested it
against dozens of bacterial strains isolated from patients and grown
in lab dishes, and found that it was able to kill many that are
resistant to treatment, including,
The drug worked against
every species that they tested, with the exception of
Pseudomonas aeruginosa, a difficult-to-treat lung pathogen.
To test halicin's effectiveness in living animals, the researchers
used it to treat mice infected with A. baumannii, a bacterium that
has infected many U.S. soldiers stationed in Iraq and Afghanistan.
The strain of A.
baumannii that they used is resistant to all known antibiotics, but
application of a halicin-containing ointment completely cleared the
infections within 24 hours.
Preliminary studies suggest that halicin kills bacteria by
disrupting their ability to maintain an electrochemical gradient
across their cell membranes.
This gradient is
necessary, among other functions, to produce
ATP (molecules that
cells use to store energy), so if the gradient breaks down, the
cells die.
This type of killing
mechanism could be difficult for bacteria to develop resistance to,
the researchers say.
"When you're dealing
with a molecule that likely associates with membrane components,
a cell can't necessarily acquire a single mutation or a couple
of mutations to change the chemistry of the outer membrane.
Mutations like that
tend to be far more complex to acquire evolutionarily," Stokes
says.
In this study, the
researchers found that E. coli did not develop any resistance to
halicin during a 30-day treatment period.
In contrast, the bacteria
started to develop resistance to the antibiotic ciprofloxacin within
one to three days, and after 30 days, the bacteria were about 200
times more resistant to ciprofloxacin than they were at the
beginning of the experiment.
The researchers plan to pursue further studies of halicin, working
with a pharmaceutical company or nonprofit organization, in hopes of
developing it for use in humans.

Universal History Archive
Universal Images Group
via Getty Images
Optimized
molecules
After identifying halicin, the researchers also used their model to
screen more than 100 million molecules selected from the ZINC15
database, an online collection of about 1.5 billion chemical
compounds.
This screen, which took
only three days, identified 23 candidates that were structurally
dissimilar from existing antibiotics and predicted to be nontoxic to
human cells.
In laboratory tests against five species of bacteria, the
researchers found that eight of the molecules showed antibacterial
activity, and two were particularly powerful. The researchers now
plan to test these molecules further, and also to screen more of the
ZINC15 database.
The researchers also plan to use their model to design new
antibiotics and to optimize existing molecules.
For example, they could
train the model to add features that would make a particular
antibiotic target only certain bacteria, preventing it from killing
beneficial bacteria in a patient's digestive tract.
"This groundbreaking
work signifies a paradigm shift in antibiotic discovery and
indeed in drug discovery more generally," says Roy Kishony, a
professor of biology and computer science at
Technion (the
Israel Institute of Technology), who was not involved in the
study.
"Beyond in silica
screens, this approach will allow using deep learning at all
stages of antibiotic development, from discovery to improved
efficacy and toxicity through drug modifications and medicinal
chemistry."
The research was funded
by,
-
the Abdul Latif
Jameel Clinic for Machine Learning in Health
-
the Defense
Threat Reduction Agency
-
the Broad
Institute
-
the
DARPA Make-It
Program
-
the Canadian
Institutes of Health Research
-
the Canadian
Foundation for Innovation
-
the Canada
Research Chairs Program
-
the Banting
Fellowships Program
-
the Human
Frontier Science Program
-
the Pershing
Square Foundation
-
the Swiss
National Science Foundation
-
a National
Institutes of Health Early Investigator Award
-
the National
Science Foundation Graduate Research Fellowship Program
-
a gift from Anita
and Josh Bekenstein
|